Neonatology
Chief, Department of Neonatology
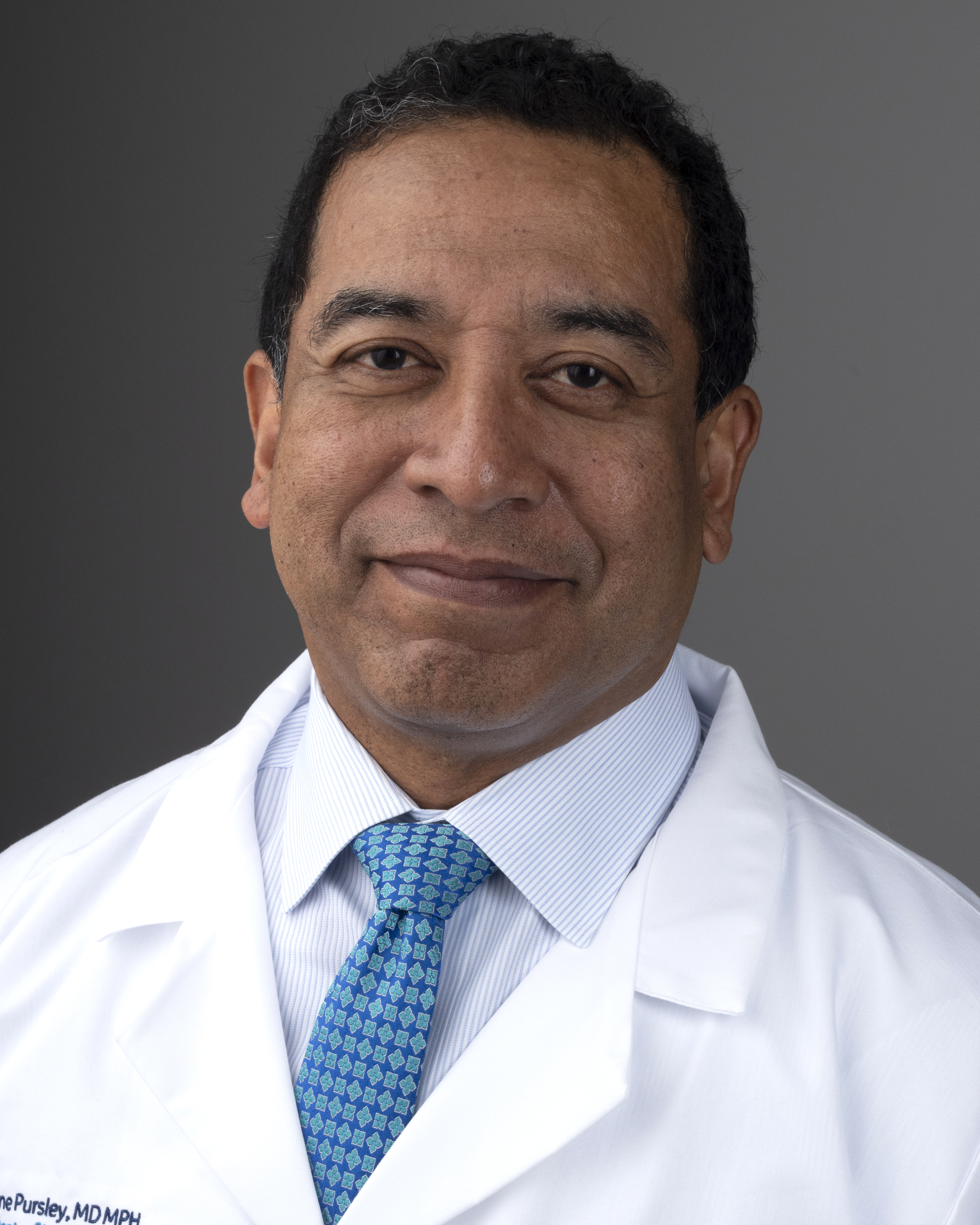
DeWayne Pursley, MD, MPH
Chief of Neonatology at Beth Israel Deaconess Medical Center
DeWayne Pursley, MD, MPH, is chief of the BIDMC Department of Neonatology, and medical director of the Klarman Family Neonatal Intensive Care Unit (NICU). He is Associate Professor of Pediatrics at Harvard Medical School (HMS) and associate clinical chief of the Boston Children’s Hospital (BCH) Division of Newborn Medicine.
Dr. Pursley currently serves as chair of the board of directors of the American Board of Pediatrics and on the American Academy of Pediatrics NICU Verification committee, which recently established national standards for risk appropriate NICU care. At HMS Dr. Pursley serves as chair of the Financial Aid Committee and as a member of the Promotion and Review Board.


DeWayne Pursley, MD, MPH, is chief of the BIDMC Department of Neonatology, and medical director of the Klarman Family Neonatal Intensive Care Unit (NICU). He is Associate Professor of Pediatrics at Harvard Medical School (HMS) and associate clinical chief of the Boston Children’s Hospital (BCH) Division of Newborn Medicine.
Dr. Pursley currently serves as chair of the board of directors of the American Board of Pediatrics and on the American Academy of Pediatrics NICU Verification committee, which recently established national standards for risk appropriate NICU care. At HMS Dr. Pursley serves as chair of the Financial Aid Committee and as a member of the Promotion and Review Board.



About Neonatology
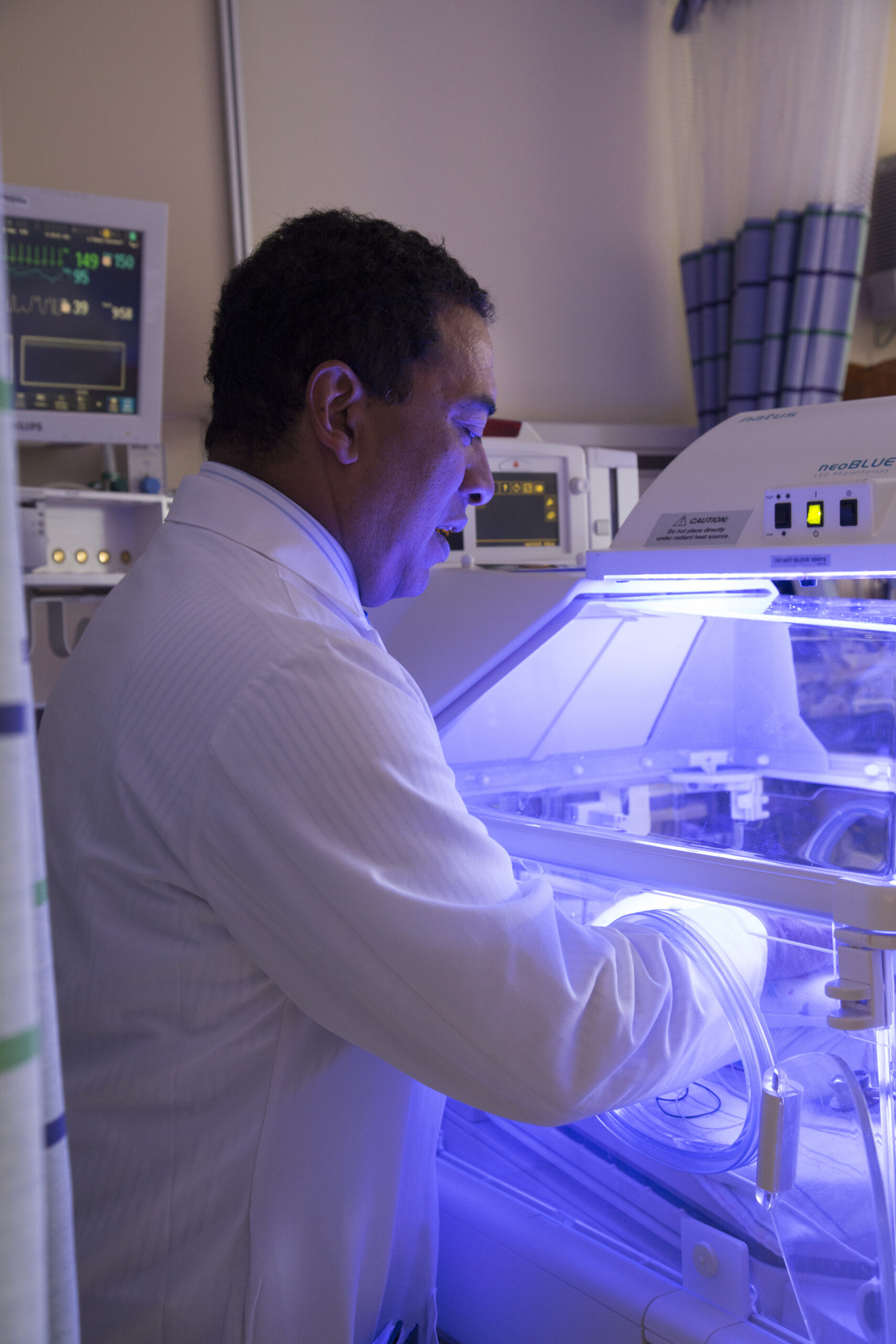
Harvard Medical Faculty Physicians at Beth Israel Deaconess Medical Center's (HMFP) Department of Neonatology is responsible for all clinical and academic activity related to newborns. Each year, the Neonatology faculty, affiliated with Harvard Medical School (HMS), provides care to more than 1,000 inborn and outborn patients in the neonatal intensive care unit, and 4,500 well newborns at BIDMC. The Department of Neonatology is also responsible for care at the special care nurseries at other BILH and affiliated hospitals.
The department includes academic physicians, general pediatricians, and neonatal hospitalists, and advanced practice providers. Our commitment to deliver exceptional patient care is further supported by more than 300 Boston Children’s Hospital medical and surgical subspecialists. Neonatology faculty include nationally recognized leaders in clinical innovation, quality improvement, medical education, and clinical and translation research in health services, implementation science, and health equity.


Providing Clinical Excellence in Neonatology
HMFP Neonatology faculty, actively engaged in high level education and research, and the multi-disciplinary NICU team provide an extensive range of clinical services in the 62-bed Klarman Family Newborn Intensive Care Unit. In addition to serving high risk neonatal patients born at BIDMC and transferred from BILH and affiliated hospitals, our team also cares for newborns in the Postpartum Newborn Unit.
Department Links



Departments
Harvard Medical Faculty Physicians at Beth Israel Deaconess Medical Center (HMFP) includes 13 specialty clinical departments. HMFP has more than 2,200 specialty physicians and advanced practice professionals, providing services across the Beth Israel Lahey Health (BILH) system, and other hospitals across eastern Massachusetts. To learn more about a specific department, click below.